-
Foodborne illnesses caused by various microorganisms, such as viruses, bacteria, and parasites (1), pose a significant global public health threats, leading to widespread illness and mortality. A survey conducted on the burden of acute gastrointestinal infections (AGI) in China between 2014 and 2015 revealed a population prevalence of 2.3% with an annual incidence of 0.3 episodes per person (2). Over the decade from 2010 to 2020, there were 18,331 reported outbreaks in Chinese catering facilities, resulting in 206,718 illnesses, 68,561 hospitalizations, and 201 fatalities (3). The Beijing CDC initiated a foodborne disease surveillance system in 2013, gradually implementing city-wide population-based surveillance. This study examined data from 36 actively monitored hospitals (25 tertiary-level and 11 secondary-level hospitals) selected through probability proportional to size (PPS) sampling from all hospitals with enteric disease clinics across 16 districts in Beijing Municipality, China.
Patients included in the surveillance were those who visited the sentinel hospital with symptoms of suspected foodborne diarrhea, presenting with over three bowel movements in 24 hours and abnormal stool consistency (e.g., loose, liquid, mucous, or bloody stools), excluding cases linked to antibiotic use or chemical exposure. Surveillance was carried out year-round, with each district aiming to collect a minimum of 330 samples annually.
Fresh stool specimens were collected either in fecal containers or rectal swabs, which were then placed in Cary-Blair transport medium for testing within 24 hours at 4°C (samples forVibrio parahaemolyticuswere stored at room temperature). Virus detection samples not immediately sent were stored at −20 °C. Bacterial specimens were enriched, inoculated onto suitable media for culture, and then isolated. Virus detection was conducted through nucleic acid amplification using reverse transcription-polymerase chain reaction (RT-PCR).
The 36 sentinel hospitals were responsible for gathering demographic information, food history, clinical characteristics, and biological samples from individuals under surveillance. A total of 16 district CDC laboratories tested these specimens for major foodborne pathogens:Salmonella,Vibrio parahaemolyticus, diarrheagenicEscherichia coli(DEC),Shigella, and Norovirus. The detection results were then sent to higher authorities for confirmation. Surveillance data indicated that Norovirus and DEC were the predominant pathogens, individuals between 19 and 30 years old had the highest infection rates, and patients withSalmonellainfections were more likely to experience fever symptoms.
Summary statistics, including frequencies and proportions, were computed for categorical variables. The study period was stratified into two time frames, 2013–2017 and 2018–2023, due to changes in testing practices at sentinel hospitals in 2018. The chi-square test was employed to compare demographic characteristics (age, sex, area, and occupation) for four pathogens (Salmonella, Norovirus,Vibrio parahaemolyticus, and DEC);Shigellawas excluded due to a limited sample size. Fisher’s exact test was used if the conditions for the chi-square test were not met. All tests were two-sided, and a significance level ofP<0.05 was considered statistically significant.
From January 1, 2013, to December 31, 2023, a total of 60,223 patients were included in the Beijing Foodborne Disease Active Surveillance System. After excluding non-infectious diarrhea cases and those without biological samples, 57,021 specimens were analyzed forSalmonella,Shigella,Vibrio parahaemolyticus, DEC, and Norovirus. The detection rates forSalmonella,Shigella,Vibrio parahaemolyticus, and DEC were 3.96% (2,260/57,021), 0.18% (101/57,021), 3.18% (1,811/57,021), and 7.06% (4,024/57,021), respectively. Among the 23,506 specimens tested for Norovirus, the detection rate was 10.54% (2,478/23,506). The prevalentSalmonellaserotypes wereSalmonellaEnteritidis (864/2,260) andSalmonellaTyphimurium (340/2,260). EnteroaggregativeEscherichia coli(EAEC) and enterotoxigenicEscherichia coli(ETEC) were the most common DEC types, constituting 34.57% (1,391/4,026) and 34.09% (1,372/4,026) of the detected DEC, respectively.
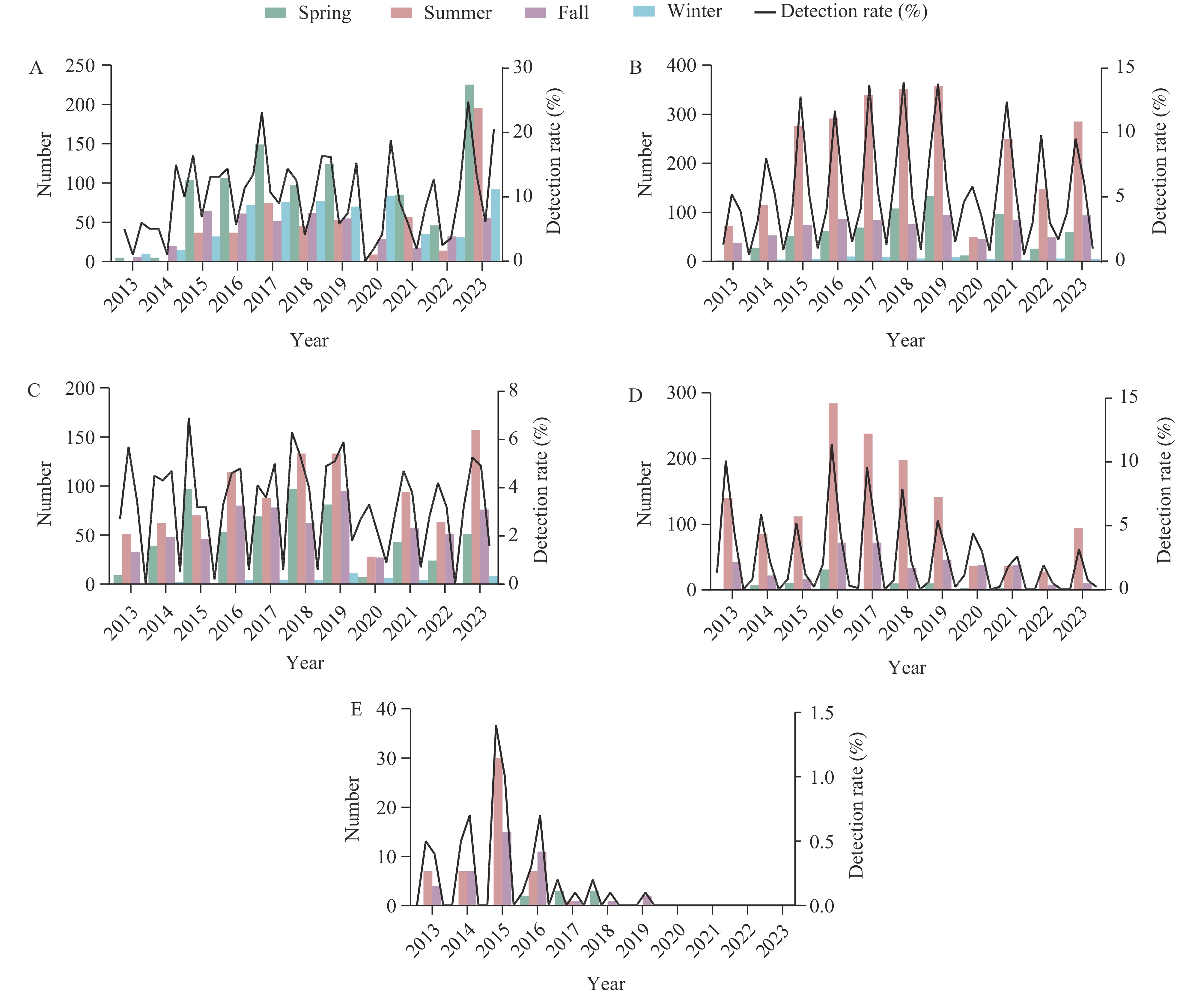
The trends in detection rates of various pathogens from 2013 to 2023 were analyzed and shown inFigure 1. From 2013 to 2019,Salmonella, DEC, and Norovirus infection rates increased annually, whileShigellainfections decreased.Vibrio parahaemolyticuspeaked in 2016, followed by a yearly decline. During 2020–2022, all pathogen infection rates decreased due to the impact of the COVID-19 pandemic. However, in 2023, detection rates increased for all pathogens exceptShigella. Notably, pathogenic bacteria were most prevalent in summer, with Norovirus causing winter and spring outbreaks.
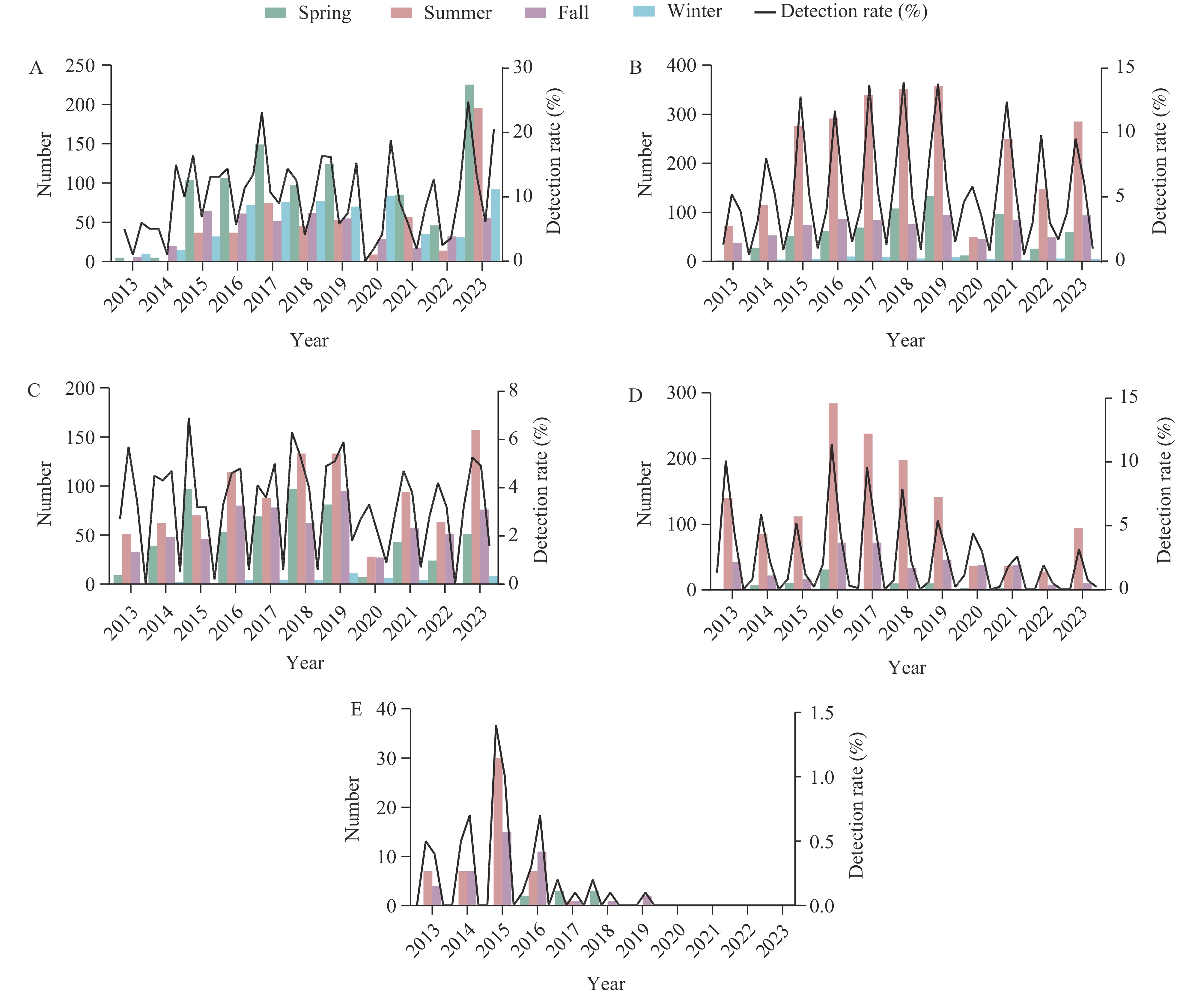 Figure 1.
Figure 1.Changes in the numbers of positive pathogens and detection rates by pathogen and season in Beijing Municipality, China, from 2013 to 2023. (A) Norovirus; (B) DEC; (C)Salmonella; (D)Vibrio parahaemolyticus; (E)Shigella.
Abbreviation: DEC=diarrhoeagenic Escherichia coli.The study provides a summary and comparison of the epidemiological characteristics of pathogens over time (Table 1). A high percentage of patients, 28.38% (2,971/10,469), are aged 19–30 years. The incidence ofVibrio parahaemolyticusinfection is significantly lower in children under 3 years old compared to other age groups (P<0.001). Gender ratios of individuals infected with Norovirus, DEC,Salmonella, andVibrio parahaemolyticusshow no significant differences between the periods 2013–2017 and 2018–2023 (P>0.05). However, there are notable disparities in the regional distribution of Norovirus (P<0.001) andSalmonella(P=0.003) infections between these time frames, with urban infections being more common in 2018–2023 compared to 2013–2017. The majority of Norovirus cases involve official staff (25.00%–29.62%), while cases of DEC,Salmonella, andVibrio parahaemolyticuspredominantly affect unemployed individuals (17.00%–28.77%). Significant differences exist in the occupational distribution of infection rates for different pathogens in different periods (P<0.001).
Variables Total Norovirus Pvalue DEC Pvalue Salmonella Pvalue Vibrio parahaemolyticus Pvalue 2013–
20232013–
20172018–
20232013–
20172018–
20232013–
20172018–
20232013–
20172018–
2023Total 10,469 888 1,590 1,671 2,353 948 1,312 1,140 671 Age, years 0.003 <0.001 <0.001 <0.001 ≤3 873
(8.34)98
(11.04)156
(9.81)131
(7.84)214
(9.09)73
(7.70)219
(16.70)4
(0.35)2
(0.36)4–18 674
(6.44)61
(6.87)83
(5.22)77
(4.61)176
(7.48)63
(6.65)131
(9.98)39
(3.42)21
(3.13)19–30 2,971
(28.38)292
(32.89)466
(29.31)498
(29.80)571
(24.27)236
(24.90)236
(17.99)467
(40.96)239
(35.62)31–40 2,303
(22.00)179
(20.16)405
(25.47)325
(19.45)565
(24.01)179
(18.89)212
(16.16)268
(23.51)223
(33.23)41–50 1,100
(10.51)75
(8.45)156
(9.81)165
(9.87)246
(10.45)129
(13.61)132
(10.06)147
(12.89)75
(11.18)51–60 1,038
(9.91)98
(11.04)113
(7.11)214
(12.81)213
(9.05)101
(10.65)144
(10.98)97
(8.51)61
(9.09)≥60 1,510
(14.42)85
(9.57)211
(13.27)261
(15.62)368
(15.64)167
(17.62)238
(18.14)118
(10.35)50
(7.45)Sex 0.934 0.210 0.492 0.535 Male 5,759
(55.00)492
(55.41)913
(57.42)887
(53.08)1,296
(55.08)497
(52.43)707
(55.89)644
(56.49)369
(55.00)Female 4,710
(45.00)396
(44.59)677
(42.58)784
(46.92)1,057
(44.92)451
(47.57)605
(46.11)496
(43.51)302
(45.00)Area <0.001 0.262 0.003 0.005 Urban 4,250
(40.81)314
(35.36)706
(45.23)716
(42.85)953
(40.69)355
(37.45)583
(44.54)474
(41.58)257
(38.36)Suburbs 4,018
(38.59)403
(45.38)637
(40.81)557
(33.33)784
(33.48)400
(42.19)486
(37.13)444
(38.95)310
(46.27)Outskirts 2,145
(20.60)171
(19.26)218
(13.97)398
(23.82)605
(25.83)193
(20.36)240
(18.33)222
(19.47)103
(15.37)Occupation 0.002 <0.001 <0.001 0.022 Official staff 2,438
(23.29)222
(25.00)471
(29.62)367
(21.96)515
(21.89)181
(19.09)159
(15.59)295
(25.88)188
(28.02)Unemployed 2,262
(21.61)151
(17.00)303
(19.06)388
(23.22)450
(19.12)224
(23.63)219
(21.47)328
(28.77)175
(26.08)Student 987
(9.43)97
(10.92)169
(10.63)139
(8.32)259
(11.01)71
(7.49)79
(7.75)80
(7.02)33
(4.92)Children 1,048
(10.01)102
(11.49)176
(11.07)137
(8.20)255
(10.84)102
(10.76)279
(21.27)14
(1.23)2
(0.35)Worker 663
(6.33)55
(6.19)77
(4.84)102
(6.10)149
(6.33)57
(6.01)69
(5.26)102
(8.95)71
(10.58)Retirees 1,168
(11.16)83
(9.35)169
(10.63)253
(15.14)284
(12.07)113
(11.92)159
(12.19)85
(7.46)38
(5.67)Others 1,903
(18.18)178
(20.05)225
(14.15)285
(17.06)441
(18.74)200
(21.10)195
(14.86)236
(20.70)164
(24.44)Abbreviation: DEC=diarrhoeagenicEscherichia coli. Table 1.Variations in demographic characteristics of foodborne diarrhea patients over select time periods in Beijing Municipality, China, 2013–2023,n(%).
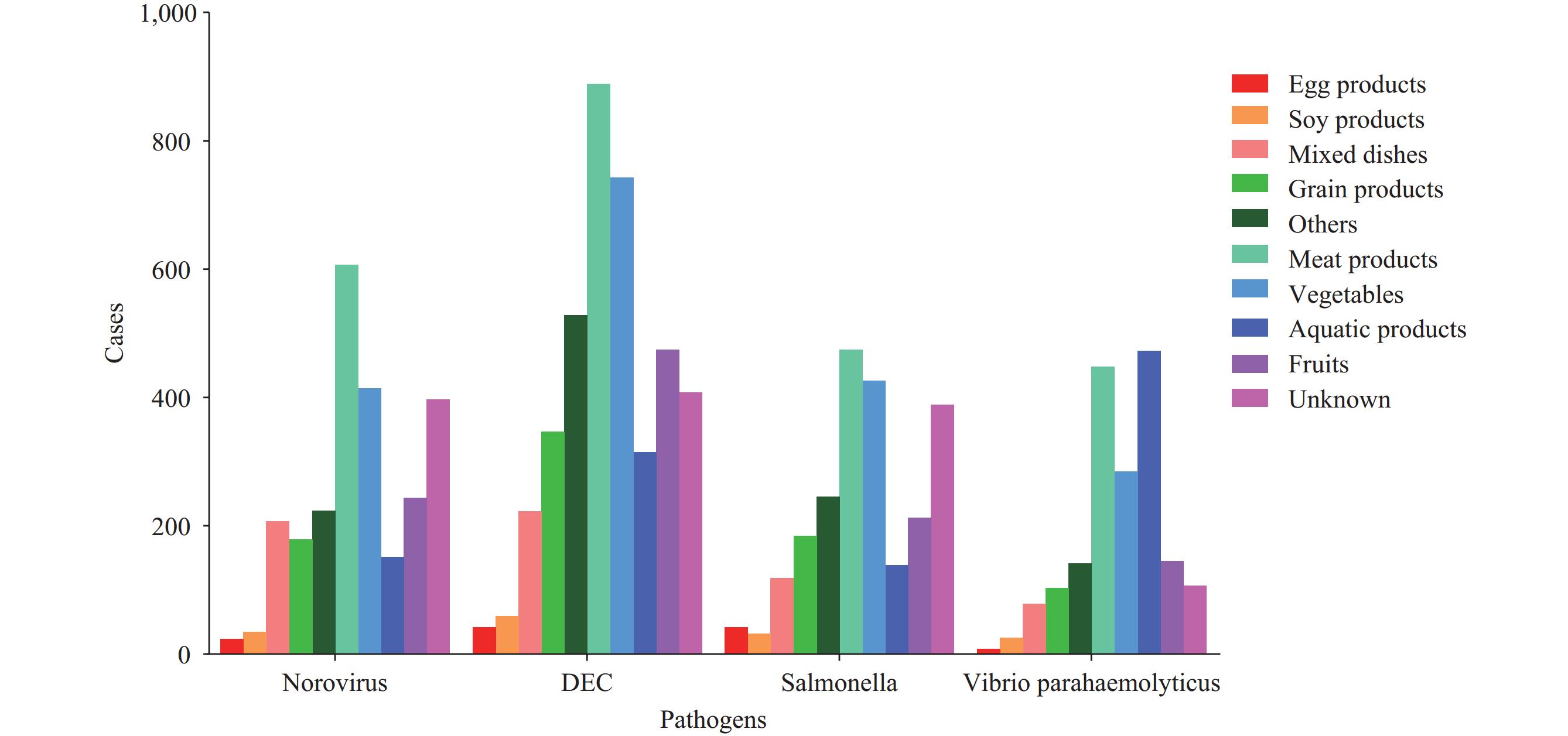
Figure 2displays patient self-reports, indicating that meat products were the most commonly reported source of suspected exposure among the four pathogens analyzed, accounting for 22.64%. However, there were differences in the distribution of suspicious food categories across the various pathogens. ForVibrio parahaemolyticusinfections, aquatic products were the primary food source at 26.06%, followed by meat products at 24.74% and vegetables at 15.74%. Conversely, patients infected with Norovirus,Salmonella, and DEC identified meat products and vegetables as the top two food sources.
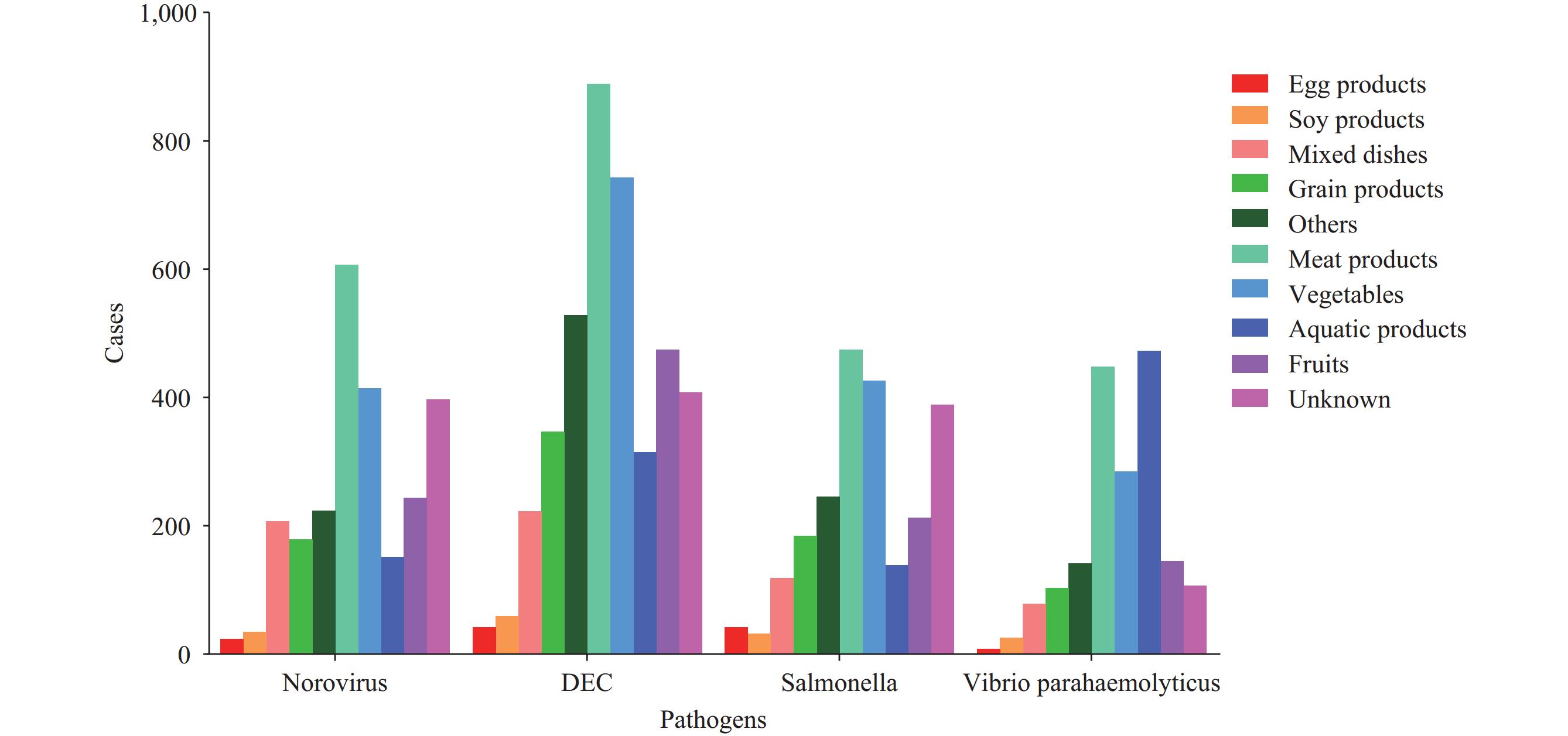 Figure 2.
Figure 2.Distribution of suspicious food categories by pathogens in Beijing Municipality, China, 2013–2023.
Abbreviation: DEC=diarrhoeagenic Escherichia coli.The clinical characteristics of the pathogens are outlined (Table 2). Nausea was the most common symptom, affecting 51.05% (1,265/2,478) of Norovirus-infected patients. Abdominal cramps were prevalent in DEC,Salmonella, andVibrio parahaemolyticusinfections, ranging from 41.08% to 73.86%.Salmonellainfections showed a significantly higher fever prevalence (36.02%) compared to other pathogens during 2013–2023. Across eleven years, the proportion of abdominal cramps from these infections decreased notably from 53.72%–73.86% (2013–2017) to 40.63%–56.93% (2018–2023). The projected trend suggests an increase in patients experiencing loose stools due to pathogens, expected to rise from 16.75%–28.27% (2013–2017) to 35.32%–45.90% (2018–2023).
Variables Total Norovirus DEC Salmonella Vibrio parahaemolyticus Pvalue* 2013–
2023Total 2013–
20172018–
2023Total 2013–
20172018–
2023Total 2013–
20172018–
2023Total 2013–
20172018–
2023Total 10,469 2,478 888 1,590 4,024 1,671 2,353 2,260 948 1,312 1,811 1,140 671 Clinical symptom Nausea 4,778
(45.64)1,265
(51.05)487
(54.84)778
(48.93)1,654
(41.10)779
(46.62)875
(37.19)856
(37.88)401
(42.30)455
(34.68)1,143
(63.11)727
(63.77)416
(62.00)<0.001 Vomiting 3,023
(28.88)965
(38.94)354
(39.86)611
(38.43)936
(23.26)414
(24.78)522
(22.18)469
(20.75)208
(21.94)261
(19.89)771
(42.57)493
(43.25)278
(41.43)<0.001 Abdominal cramps 5,542
(52.94)1,123
(45.32)477
(53.72)646
(40.63)2,123
(53.76)1,061
(63.49)1,062
(45.13)1,142
(50.53)603
(63.61)539
(41.08)1,224
(67.59)842
(73.86)382
(56.93)<0.001 Fever
(≥37.5 °C)2,481
(23.70)452
(18.24)201
(22.64)251
(15.79)783
(19.46)424
(25.37)359
(15.26)814
(36.02)357
(37.66)457
(34.83)400
(22.09)281
(24.65)119
(17.73)<0.001 Dehydration 785
(7.50)223
(9.00)88
(9.91)135
(8.49)208
(5.17)102
(6.10)106
(4.50)188
(8.32)89
(9.39)99
(7.55)176
(9.72)119
(10.44)57
(8.49)<0.001 Thirsty 1,365
(13.04)245
(9.89)143
(16.10)102
(6.42)288
(7.16)169
(10.11)119
(5.06)196
(8.67)136
(14.35)60
(4.57)207
(11.43)163
(14.30)44
(6.56)<0.001 Fatigue 1,253
(13.67)302
(12.19)118
(13.29)184
(11.57)453
(11.26)212
(12.69)241
(10.24)291
(12.88)159
(16.77)132
(10.06)326
(18.00)236
(20.70)90
(13.41)<0.001 Chills 54
(0.52)8
(0.32)5
(0.56)3
(0.19)9
(0.22)2
(0.12)7
(0.30)13
(0.58)4
(0.42)9
(0.69)26
(1.44)17
(1.49)9
(1.34)<0.001 Diarrhea frequency ≥10/24 h 2,037
(19.46)433
(17.48)144
(16.22)289
(18.18)683
(16.97)277
(16.58)406
(17.25)583
(25.80)227
(23.95)356
(27.13)341
(18.83)202
(17.72)139
(20.72)<0.001 Diarrhea Watery stool 5,936
(56.70)1,464
(59.08)510
(57.43)954
(60.00)2,082
(51.74)951
(56.91)1,131
(48.07)1,324
(58.58)584
(61.60)740
(56.40)1,159
(64.00)773
(67.81)386
(57.53)<0.001 Loose stool 3,335
(31.86)824
(33.25)251
(28.27)573
(36.04)1,468
(36.48)388
(23.22)1,080
(45.90)650
(28.76)175
(18.46)475
(36.20)428
(23.63)191
(16.75)237
(35.32)0.690 Mucus stool 518
(4.95)88
(3.56)54
(6.08)34
(2.14)175
(4.35)108
(6.46)67
(2.85)146
(6.46)88
(9.28)58
(4.42)94
(5.19)68
(5.96)26
(3.87)0.990 Rice-water stool 75
(0.72)12
(0.48)9
(1.01)3
(0.19)50
(1.24)47
(2.81)3
(0.13)6
(0.27)5
(0.53)1
(0.08)7
(0.39)5
(0.44)2
(0.30)<0.001 Pus and blood stool 66
(0.63)5
(0.20)1
(0.11)4
(0.25)24
(0.60)14
(0.84)10
(0.42)17
(0.75)9
(0.95)8
(0.61)18
(1.00)11
(0.96)7
(1.04)0.137 Abbreviation: DEC=diarrhoeagenicEscherichia coli. Table 2.Reported signs and symptoms of patients infected with different pathogens in Beijing Municipality, China, 2013–2023,n(%).
-
This continuous pathogenic surveillance study examined the incidence of foodborne diseases among outpatients with diarrhea in Beijing. Through comprehensive laboratory testing for four intestinal pathogens and one virus, the study revealed the epidemiological and pathogenic characteristics of foodborne diarrhea in the population, contributing valuable data to the understanding of such diseases in China. Over the past eleven years, 57,021 biological samples were tested for four common intestinal pathogens, while 23,506 samples were specifically tested for a single virus. Norovirus emerged as the most frequently detected pathogen, with a detection rate of 10.54%, aligning with studies conducted in Shanghai Municipality and Zhejiang Province, confirming that norovirus infection is the leading cause of diarrhea in these regions (4–5). Noroviruses are the primary etiological agents responsible for sporadic cases and outbreaks of acute gastroenteritis globally, imposing a substantial disease burden in both developed and developing nations. Currently, most outbreaks under surveillance in China are large-scale, while smaller clusters also constitute a significant proportion. Therefore, there is a need for further enhancement in their monitoring and analysis (6). Regarding temporal distributions, the detection rates of all five pathogens decreased in 2020 due to the coronavirus disease 2019 (COVID-19) pandemic, mirroring similar observations reported in the US (7). The detection rate ofShigelladecreased annually from 2013 to 2023, consistent with a study onShigellainfection in China (8). This decline is likely due to various factors, including rapid economic growth, improved water supply systems, upgraded sanitation facilities, and heightened awareness of hygiene practices. Regarding seasonality, the detection rates of the four bacterial pathogens peaked in spring and summer, while norovirus was the main cause of winter outbreaks, consistent with previous reports (9). Among cases ofSalmonellainfection, meat products and vegetables were the most commonly implicated foods, contrary to a study in the US (10) that reported eggs as the most commonly implicated food. The most common clinical symptoms were nausea, vomiting, and abdominal cramps. Patients infected withSalmonellawere more likely to have a fever. The research on clinical symptoms provides valuable insights for clinical diagnosis. Given the atypical clinical manifestations of various pathogens, differentiating them from non-infectious diarrhea remains challenging. Therefore, there is an urgent need to establish rapid pathogen monitoring methods to enable targeted treatment strategies when patients seek medical care.
The study is subject to some limitations. The surveillance data from 36 medical institutions may not provide an accurate estimate of the overall prevalence of foodborne diseases in Beijing. While efforts were made to adhere to national standards and provide regular training, variations in results among hospitals and laboratories are possible. Moreover, reliance on self-reported food exposure information by patients can introduce recall bias, as there are no valid laboratory methods to confirm these reports.
The advancement of our economy has led to significant lifestyle transformations. The rising popularity of ready-to-eat or pre-cooked meals highlights the need for a comprehensive strategy to safeguard the entire food supply chain, from production to consumption, to safeguard consumers against foodborne diseases. Thus, we advocate for improved food safety education for at-risk groups and the implementation of proactive and efficient control measures tailored to the epidemiological patterns of foodborne diarrhea cases in Beijing.
-
No conflicts of interest.
-
All members from the participating CDCs for their contributions.
HTML
| Citation: |



 Download:
Download: