-
Chronic respiratory diseases (CRDs) pose a significant public health challenge amid the population’s accelerating aging process. Globally, tobacco smoking is the primary cause of mortality associated with CRDs (1). It is essential to understand the prevalence and characteristics of smoking among CRD patients to inform targeted smoking cessation interventions. However, existing tobacco surveillance in China is designed for the general population and does not specifically cover CRD patients (2). To bridge this gap, we analyzed electronic medical records (EMRs) to assess smoking behavior among 28,334 hospitalized CRD patients at Beijing Chao-Yang Hospital. We found that 30.7% of these patients were former smokers and 18.0% were current smokers. Notably, patients with chronic obstructive pulmonary disease (COPD) and lung cancer exhibited higher rates of smoking and greater pack-years compared to others. These findings underscore the critical need for enhanced smoking monitoring and cessation programs for hospitalized CRD patients.
We conducted a retrospective study at Beijing Chao-Yang Hospital, a premier institution for respiratory medicine in China and the facility with the highest number of respiratory disease inpatients in Beijing. This setting was ideal for surveilling smoking behaviors among hospitalized patients with CRDs. Our study included patients admitted between January 1, 2014, and December 31, 2023, with a primary discharge diagnosis of one of five CRDs classified by the International Classification of Diseases 10th Revision (ICD-10): COPD (ICD-10: J44), asthma (ICD-10: J45-J46), interstitial lung disease (ICD-10: J84), bronchiectasis (ICD-10: J47), and lung cancer (ICD-10: C34). We identified 30,129 cases of CRDs, and after excluding 1,795 cases due to missing smoking information, 28,334 cases were analyzed. The Research Ethics Board of Beijing Chao-Yang Hospital approved the study (2022-ke-221).
Smoking information was extracted from EMRs using natural language processing techniques. Physicians recorded the patients’ smoking status and habits prior to the current hospital admission during medical history consultations. Patients were classified as current smokers, former smokers, or never smokers. Current smokers were identified as those who reported active smoking at the time of admission. Former smokers were individuals who had smoked at some point but had ceased smoking before their current admission, while never smokers had no lifetime history of smoking. Respiratory symptoms observed at admission were also documented from EMRs. Hospitalization outcomes, such as prolonged hospital stays (defined as a length of stay exceeding 14 days), use of invasive mechanical ventilation, transfers to intensive care units, and in-hospital mortality, were obtained from the discharge summaries. The prevalence of current and former smokers was computed. A multivariable logistic regression model was employed to explore the relationship between smoking status and outcomes related to respiratory symptoms and overall hospitalization. All statistical analyses were conducted using Stata (version 15.1; StataCorp, College Station, TX, USA), and a significance threshold of 0.05 was used for two-tailed tests.
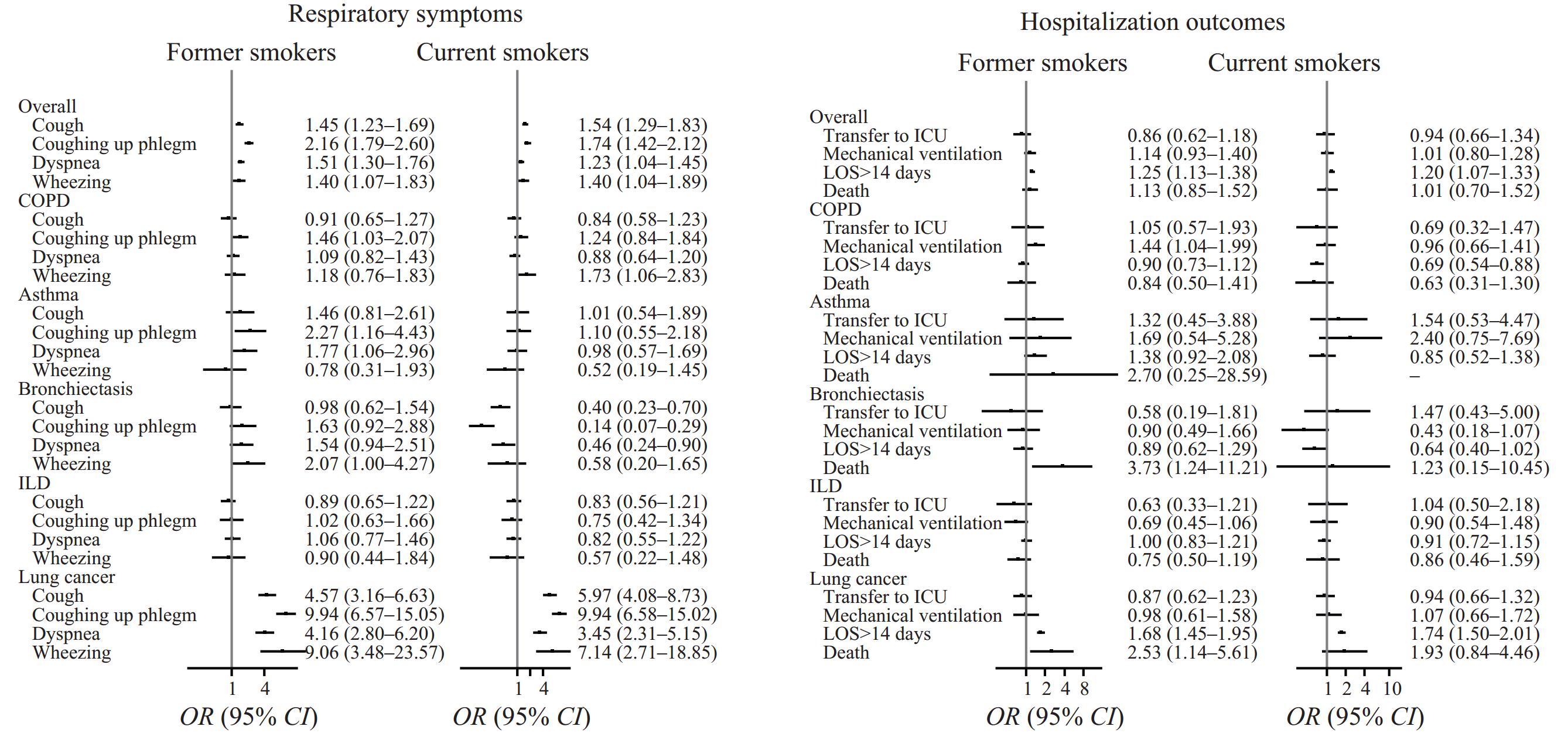
The mean age of the CRD cases included in the study was 63.6 years (standard deviation: 12.3 years), with males constituting 57.8% of the sample. The distribution of smoking status among the participants was as follows: 51.3% never smokers, 30.7% former smokers, and 18.0% current smokers. For individuals classified as ever smokers (both former and current), the median number of pack-years smoked was 30 (interquartile range: 20–50). Among former smokers, the median duration since quitting was 6 years (interquartile range: 1–12 years).Figure 1illustrates the variations in smoking prevalence by age, sex, and over time, with the highest proportion of current smokers being males aged 50–59 years (37.6%). The data further show an increasing trend in current smoking among female patients as they age. Patients suffering from COPD and lung cancer exhibited higher frequencies of smoking history and increased pack-years of smoking (Table 1).Figure 2presents the relationship between smoking status and both general and disease-specific health outcomes, indicating that compared with never smokers, both former and current smokers are at a higher risk for respiratory symptoms and experiencing prolonged hospital stays.
 Figure 1.
Figure 1.(A) Smoking status among patients hospitalized with chronic respiratory diseases from 2014 to 2023; (B) proportion of current smokers by age and sex; (C) proportion of former smokers by age and sex.
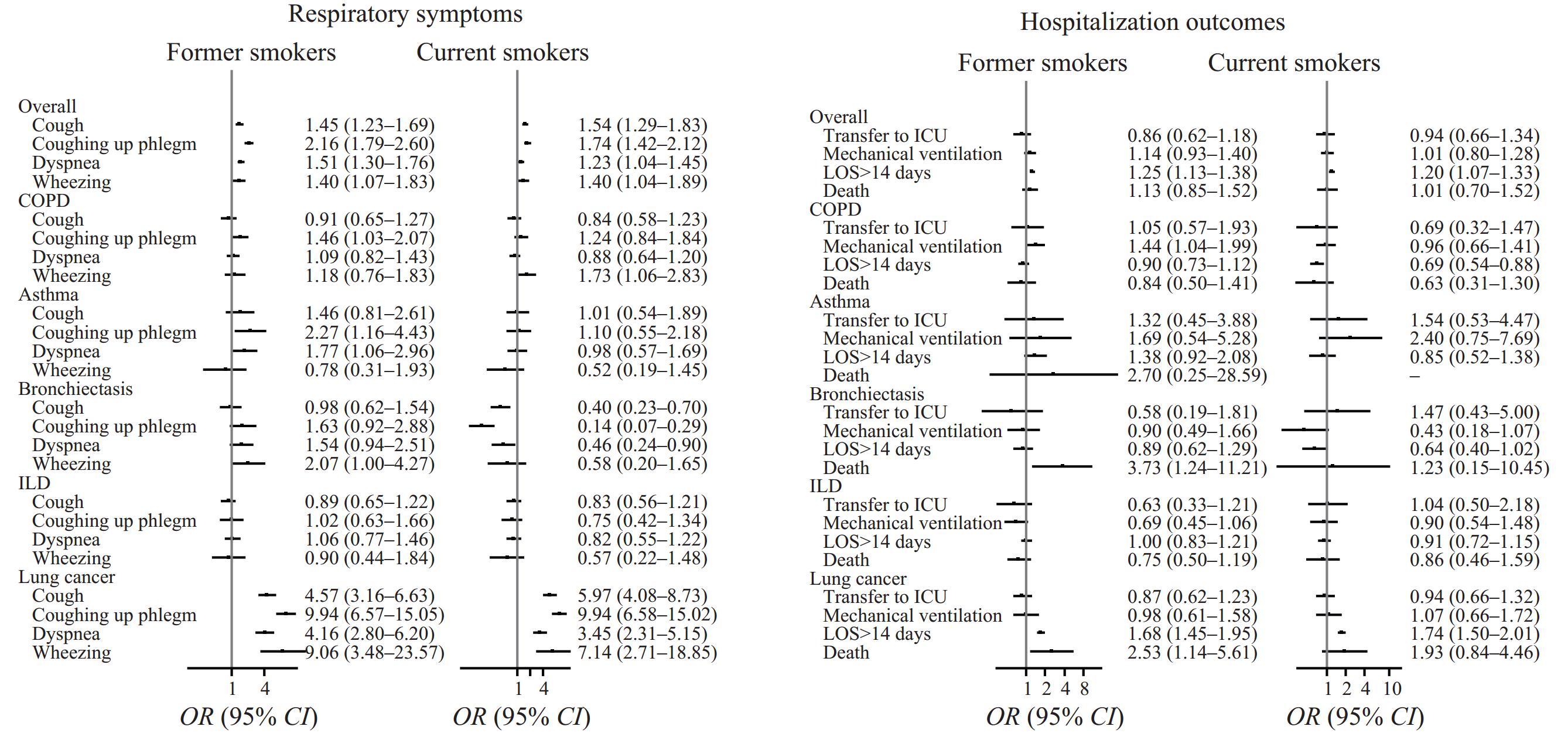 Figure 2.
Figure 2.Association between smoking status and respiratory symptoms and hospitalization outcomes.
Note: Logistic models adjusted for sex, age, disease diagnosis, diabetes history, and hypertension history. A random intercept was used to account for multiple hospitalizations of one patient. Never smokers were the reference group. Abbreviation: COPD=chronic obstructive pulmonary disease; ILD=interstitial lung disease; LOS=length of stay; ICU=intensive care unit.Characteristics Overall COPD Asthma Bronchiectasis ILD Lung cancer Total (Number) 28,334 6,089 2,676 3,214 6,763 9,592 Age (years), mean (SD) 63.6 (12.3) 71.4 (10.3) 57.5 (13.8) 60.3 (13.1) 62.3 (12.2) 62.4 (10.5) Male, Number (%) 16,382 (57.8) 4,713 (77.4) 1,134 (42.4) 1,401 (43.6) 3,644 (53.9) 5,490 (57.2) Smoking status Total Never smokers 14,524 (51.3) 1,435 (23.6) 1,767 (66.0) 2,324 (72.3) 3,847 (56.9) 5,151 (53.7) Former smokers 8,706 (30.7) 3,293 (54.1) 525 (19.6) 596 (18.5) 2,077 (30.7) 2,215 (23.1) Current smokers 5,104 (18.0) 1,361 (22.3) 384 (14.4) 294 (9.2) 839 (12.4) 2,226 (23.2) Pack-years*, M (Q25–Q75)* 30 (20–50) 40 (20–50) 20 (10–40) 23 (10–40) 30 (15–45) 40 (20–50) Men Never smokers 3,797 (23.2) 579 (12.3) 360 (31.7) 594 (42.4) 960 (26.3) 1,304 (23.7) Former smokers 7,945 (48.5) 2,941 (62.4) 449 (39.6) 544 (38.8) 1,925 (52.8) 2,086 (38.0) Current smokers 4,640 (28.3) 1,193 (25.3) 325 (28.7) 263 (18.8) 759 (20.8) 2,100 (38.3) Pack-years*, M (Q25–Q75)* 35 (20–50) 40 (22–60) 25 (10–40) 25 (10–40) 30 (18–45) 40 (22–50) Women Never smokers 10,727 (89.7) 856 (62.2) 1,407 (91.3) 1,730 (95.4) 2,887 (92.5) 3,847 (93.8) Former smokers 761 (6.4) 352 (25.6) 76 (4.9) 52 (2.9) 152 (4.9) 129 (3.1) Current smokers 464 (3.9) 168 (12.2) 59 (3.8) 31 (1.7) 80 (2.6) 126 (3.1) Pack-years*, M (Q25–Q75)* 17 (7–30) 20 (10–37) 10 (4–20) 15 (10–20) 15 (5–30) 20 (7–35) Abbreviation: COPD=chronic obstructive pulmonary disease; ILD=interstitial lung disease.
* In former and current smokers.Table 1.Demographics and smoking status of patients hospitalized with respiratory diseases.
-
In this decade-long EMR-based investigation, the prevalence of current and former smoking was significantly elevated, especially among patients diagnosed with COPD and lung cancer. The analysis highlighted that individuals with any history of smoking, including those who had quit, exhibited increased risks of respiratory symptoms and prolonged hospitalizations. These results emphasize the urgent need for specialized interventions and improved surveillance of smoking habits in hospitalized individuals with CRD and a history of smoking.
Smoking is the primary risk factor for CRDs and significantly impacts patient outcomes, contributing to 71.1% of CRD-related deaths in men and 21.9% in women in China (3). While there has been limited comprehensive analysis of smoking habits among hospitalized CRD patients, previous studies mostly utilized active surveillance (4), which is not feasible on a large scale. Employing EMR to monitor smoking behavior in this demographic offers an effective alternative, particularly for CRDs that can cause severe episodes necessitating hospital admission due to smoking and other triggers. This method has proven both feasible and beneficial for tracking smoking habits in hospitalized patients with CRDs. However, factors such as patient mix during hospital stays may affect EMR-based smoking status assessments. Following the coronavirus disease 2019 (COVID-19) outbreak in 2020, there was a noticeable decrease in the number of CRD hospitalizations, accompanied by an increase in the proportion of patients who have never smoked, suggesting a shift in the disease profile among hospital admissions.
The prevalence of current smoking among hospitalized patients with CRDs is markedly lower than in the general population. Specifically, 21.1% of patients aged 50–59 years are current smokers, compared to 27.8% of the general population of the same age group, and 19.8% of patients aged 60–69 years smoke, versus 25.8% in their general counterparts (5). This decrease is likely influenced by patients with CRDs, particularly former smokers, who may quit smoking due to their health conditions. The patterns of smoking prevalence age-wise in patients with CRDs reflect similar trends observed in the broader population, wherein the highest rates in men aged 50–59 years, and subsequently decrease with age. In contrast, smoking prevalence in women tends to increase as they age. These findings underscore the necessity for tailored smoking cessation programs, particularly for older female patients with CRDs.
We observed notable variations in smoking habits among patients with different respiratory conditions. Patients with COPD exhibited the highest prevalence of lifetime smoking, with most quitting by the time of hospital admission. The median cumulative smoking exposure for COPD patients was 40 pack-years, the highest amongst the groups studied. These observations align with a large multicenter cohort study in China, which found that among hospitalized COPD patients, 42.7% were former smokers, 19.6% were current smokers, and the average pack-years recorded was 39.44 (6). In contrast, patients with lung cancer displayed the highest proportion of current smokers, with only half of those who had ever smoked quitting by admission. Despite their younger ages, lung cancer patients demonstrated a cumulative smoking exposure comparable to those with COPD. Asthma patients, representing another prevalent CRD, showed both a lower proportion of smokers and fewer pack-years of smoking. The smoking status distribution among hospitalized asthma patients mirrored the findings from another multicenter study conducted in China (7).
Smoking was linked to various respiratory symptoms, particularly in lung cancer patients. Individuals who had quit smoking still exhibited an increased risk of respiratory symptoms, likely reflecting substantial cumulative lifetime smoking exposure. This highlights the need to consider both smoking pack-years and current smoking status when evaluating the health risks associated with smoking (8). Our results strongly suggest that individuals with CRDs should stop smoking as soon as possible. Notably, current smokers with bronchiectasis were at a lower risk for respiratory symptoms, a phenomenon possibly due to the “healthy smoker effect,” where only smokers in relatively better health continue smoking upon hospital admission. Smoking was also associated with longer hospital stays, though no significant differences were observed in other in-hospital outcomes. This finding is consistent with data from other patient groups (9) and may indicate a survivor bias, where smokers with more severe conditions might not survive long enough to be presented in studies.
The study is subject to some limitations. First, the use of a single-center design may impede the broader applicability of our findings. Nonetheless, our primary results align with those from multicenter studies in China, supporting the effectiveness of EMR-based smoking surveillance. Future studies should target more diverse populations to improve generalizability. Second, our dependence on self-reported smoking data from EMRs could lead to recall and reporting biases. Changes in smoking behavior during hospitalization were not counted. Third, smokers diagnosed with CRDs might display greater tolerance to symptoms such as coughing and dyspnea, potentially resulting in an underreported incidence of these respiratory symptoms among current smokers. Despite these challenges, an increased risk of respiratory symptoms was still evident in current smokers.
In conclusion, EMR data can effectively monitor the smoking status and characteristics of hospitalized patients with CRDs. Notably, a high proportion of patients with CRDs, particularly those with COPD and lung cancer, reported a history of smoking. Both current and former smokers exhibited increased respiratory symptoms and extended hospital stays. Based on these findings, we advocate for the implementation of smoking surveillance through EMRs and the development of targeted smoking cessation programs for hospitalized CRD patients. Further long-term studies are necessary to assess the benefits of smoking cessation in this patient cohort.
-
No conflicts of interest.
HTML
| Citation: |




 Download:
Download: