-
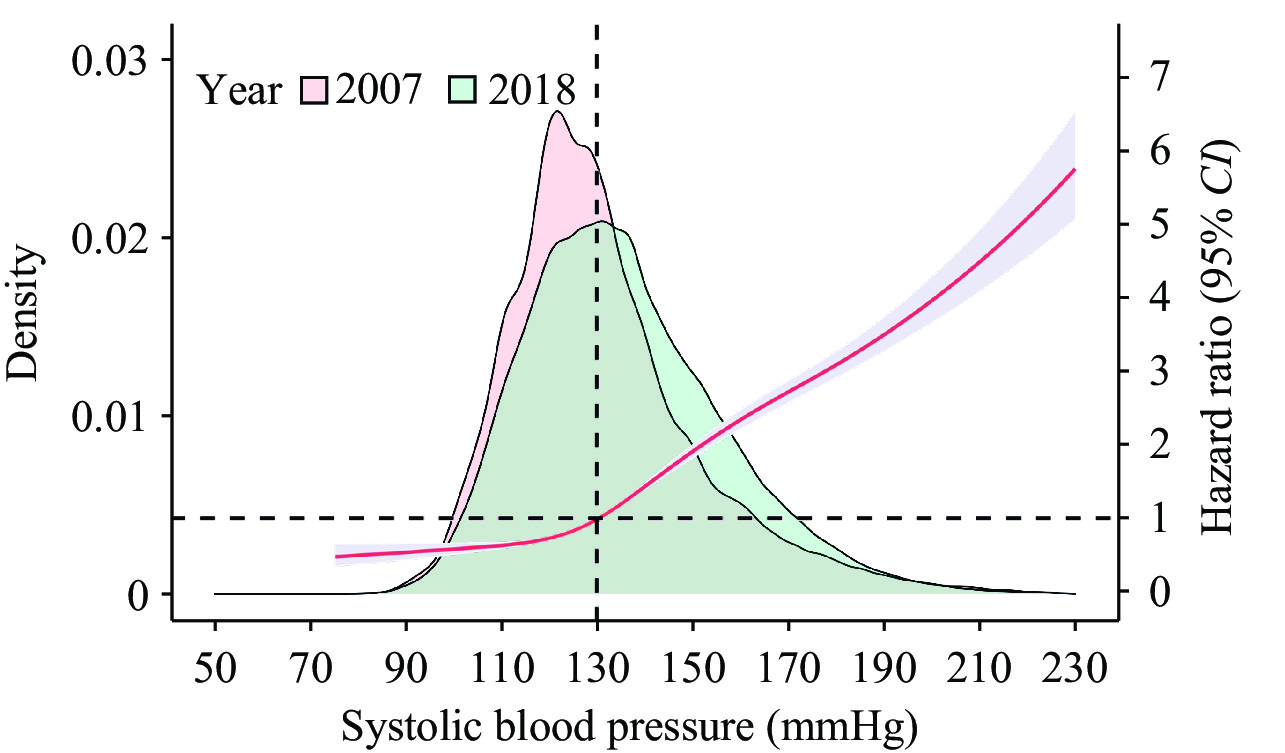
Hypertension, or high blood pressure, is a predominant precursor of premature mortality, affecting an estimated 270 million people in China alone, and is also a major global health concern (1). Hence, effective management of hypertension is vital for averting severe adverse cardiac or cerebrovascular incidents, decreasing early mortality rates, and curtailing disability. However, pharmacological treatments for hypertension demonstrate a notable variation in efficacy among individuals (2), which could partially explain the persistently low control rate of hypertension in China as observed from 2007 to 2018 (Figure 1) (3).
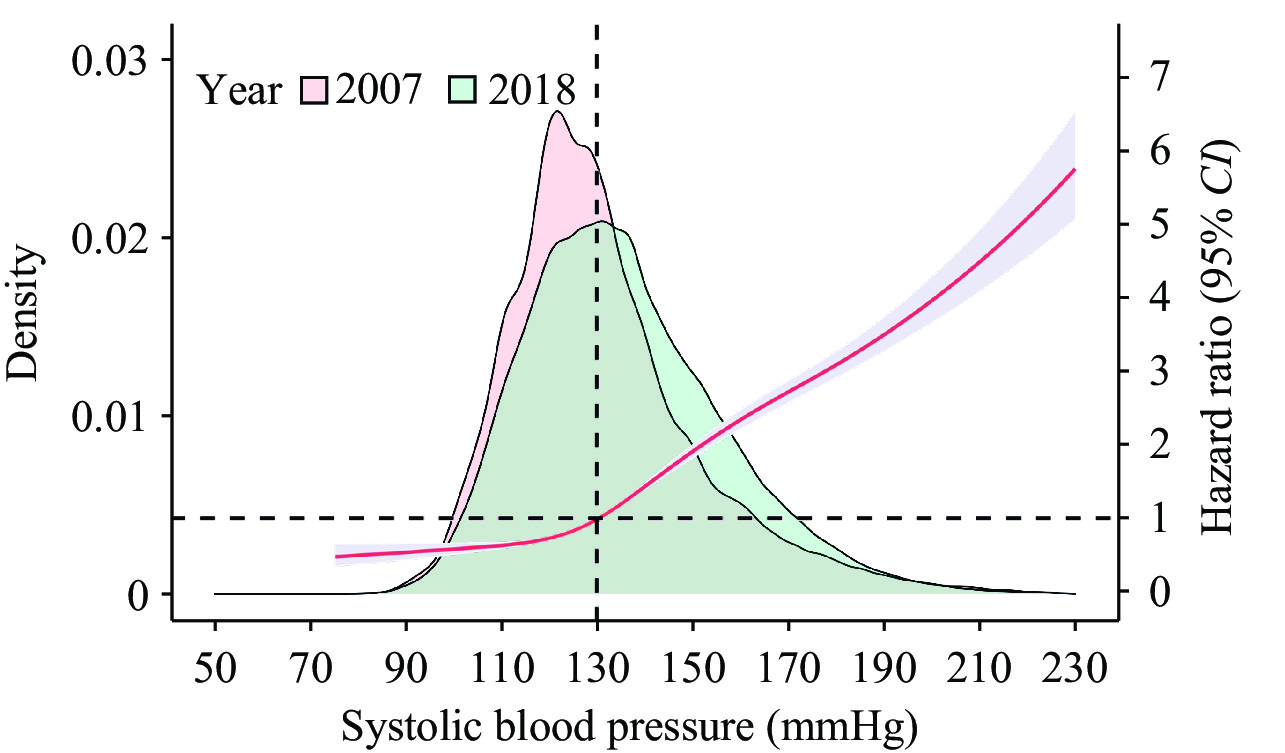 Figure 1.
Figure 1.Density plot representing systolic blood pressure in the adult population for 2007 and 2018, alongside the unadjusted hazard ratio of all-cause mortality at varying levels of systolic blood pressure with 95% confidence interval (CI).
Note: red line indicates the hazard ratio, light blue shade indicates 95%CI.
Source of data: China Chronic Disease and Risk Factor Surveillance.
Blood pressure (BP) is a heritable determinant of risk for cardiovascular and cerebrovascular diseases, with genetic predisposition to BP variation ranging from 30% to 50% (4). The genetic architecture of BP comprises more than 30 known genes (5-6). For example, polymorphic variation in the CYP2D6 gene, which encodes a cytochrome p450 family member involved in phase I drug metabolism, has been shown to influence BP response to treatments such as diuretics, beta-blockers, angiotensin receptor blockers, and clonidine (7-8).
Pharmacogenetic testing (PGx) can offer valuable insights for personalized medicine by taking into account individual variations in medicinal responses. Currently, 27 different institutions in the US are engaged in implementing pharmacogenomics programs, some of which have been operational for over a decade (9). A study titled PREPARE, which took place across seven European countries, demonstrated that genotype-guided treatment using a 12-gene pharmacogenetic panel significantly reduced the occurrence of clinically relevant adverse drug reactions (10).
Despite these promising results, the benefits of PGx remain widely debated, partly due to potential biases that might be introduced (10). Furthermore, questions remain regarding its feasibility, acceptability, and effectiveness in real-world environments. Additionally, the integration of PGx knowledge into clinical settings has been slow. There is a paramount need for the development of personalized algorithms that can aid in both the choice and management of hypertension medication, thereby incorporating PGx into standard care.
In China, numerous direct-to-consumer PGx kits can be procured via e-commerce platforms. These kits offer tailored advice on medication usage, including antihypertensives (11). Several hospitals in developed regions, such as the Fuwai Hospital of the Chinese Academy of Medical Sciences, Peking University First Hospital, Peking University People’s Hospital, and Xiangya Hospital Central South University, not to forget the Chronic Disease Prevention and Control Center of Shenzhen, have inaugurated precision medicine programs targeting major chronic ailments such as hypertension. Furthermore, initiatives like thePharmacogenomic Examination and Management ofhypertension patientsin China based on antihypertensive efficacy and adverse reactions(China-PEM), have been established to encourage the uptake of pharmacogenetic testing (12).
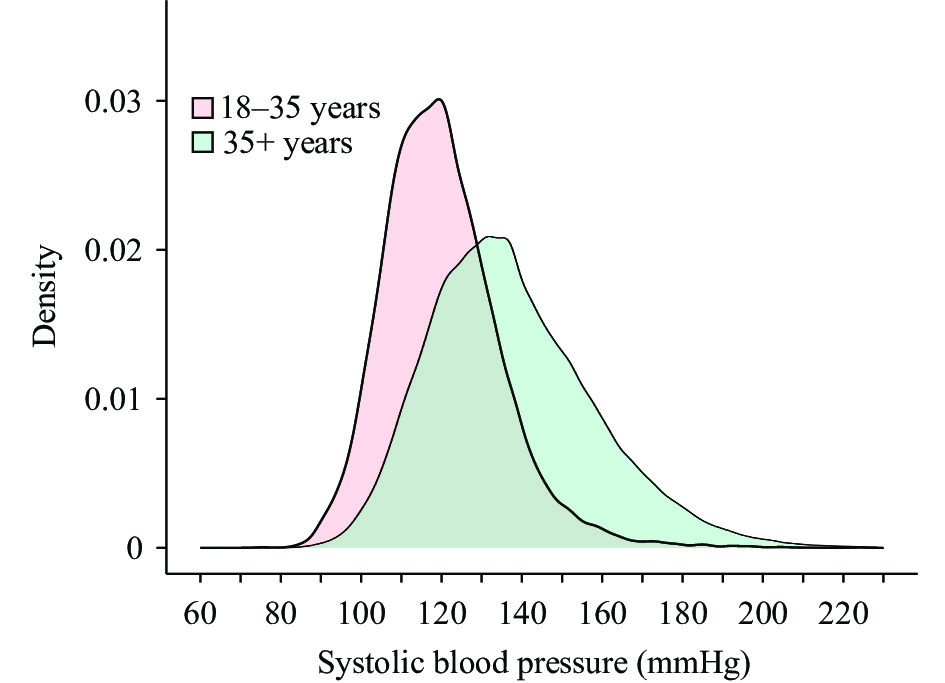
PGx presents a unique opportunity to shift from a high-risk strategy to a population-based approach for hypertension management in primary healthcare settings. Current strategies for managing hypertension in China’s primary healthcare system primarily target populations aged 35 years and older (13). However, data from the 2018 China Chronic Disease and Risk Factor Surveillance indicate that the prevalence of hypertension among individuals aged 18–34 years old has risen to 9.2%. Notably, the rates of awareness (16.0%), treatment (10.2%), and control (1.5%) in this age group significantly lag behind those of older ages (Figure 2). Although the implementation of the National Basic Public Health Service program in China has led to a hypertension control rate increase among individuals aged 18–69 years old from 5.8% to 13.7% between 2010 and 2018 (3), it remains markedly low compared to developed countries like the Republic of Korea, Canada, and Iceland (14). It is crucial to detect hypertension early in younger populations to prevent vascular aging and organ damage (15), but there is a striking lack of practical methods to draw young hypertensive patients to primary healthcare institutions for screening, diagnosis, treatment, and control. The emergence of PGx presents a viable opportunity to engage younger individuals in primary healthcare settings for the treatment and management of hypertension.
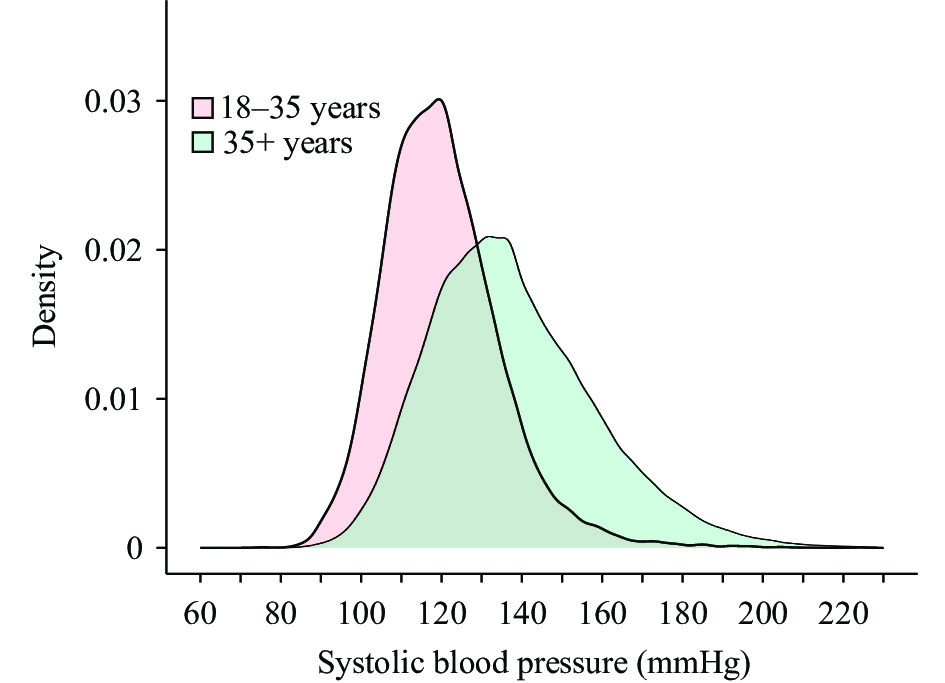 Figure 2.
Figure 2.Density plot of systolic blood pressure among adults aged 18–35 and over 35 years.
Source of data: China Chronic Disease and Risk Factor Surveillance (2018).While China has shown support for the use of PGx, there still remains a significant need for improvement in the guidelines that govern hypertension management. The State Council of China issued theMedium-to-Long Term Plan for the Prevention and Control of Chronic Diseases (2017–2025), which expressed support for the promotion and utilization of emerging technologies and products such as PGx in mitigating chronic conditions (16). Additionally, in 2022, the National Health Commission and the State Administration of Traditional Chinese Medicine issued a Notice pushing for the bolstering of drug safety management, as well as the improvement of rational drug use (17). This involved the employment of PGx to identify potential medication risks, develop personalized medication plans, optimize drug selection, and accurately determine medication dosages. The 2017Guidelines for Rational Use of Antihypertensive Drugs (2nd Edition)acknowledged the significant variance in drug responses amongst diverse individuals and advocated for the consideration of pharmacogenomics factors when prescribing antihypertensive medication. However, theNational Guideline for Hypertension Management in China (2019)and theClinical Practice Guidelines for Hypertension Management in China (2022)have yet to incorporate provisions related to the use of PGx in the administration of hypertensive treatment.
As next-generation sequencing technology continues to advance, the affordability of whole genome sequencing has significantly improved. This method has been widely adopted within China for the diagnosis and treatment of various ailments, including birth defects, malignant tumors, psychiatric disorders, and genetic metabolic disorders found in children. Several hospitals in China have developed PGx laboratories, complete with genetic counseling services.
However, there is a pressing need for an established management framework within the Chinese government. This would guide the application of PGx technology, transitioning from the discovery of novel genes to equitable health benefits for the population. Constructing an external system for appraising technical readiness levels is also critical to ensuring validity, quality, safety, and efficacy.
Further, an external quality control system should be designed for direct-to-consumer PGx testing kits. To effectively integrate PGx testing into clinical practice and avoid misinterpretation, healthcare professionals must receive thorough and detailed training. As public education and awareness campaigns are necessary for increasing understanding and acceptance of PGx testing, these too should be initiated.
Finally, integrating genetic testing into population-based surveillance can significantly augment our understanding of associations between genetics and the environment related to chronic diseases in China. This will inform the design of essential medication lists tailored to regional variations.
The advancement of PGx and precision medication presents notable obstacles in achieving health equity in clinical practice throughout the expansive regions of China. In a bid to accomplish health equity, the UK has initiated a strategy that merges precision medicine and tiered diagnosis, incorporating PGx within the framework of the National Health Service. Data suggests that the average income and educational level of PGx users is higher, concurrently creating substantial challenges when extending the application of PGx in remote and economically disadvantaged regions of China. Consequently, the establishment of a learning-oriented primary healthcare service mechanism and toolkit becomes imperative for incorporating this knowledge into practice in China.
Genetic counseling is a health service that interprets genetic findings for individuals, and can be utilized in contexts such as genotype-guided medication selection, genetic risk screening, and disease diagnosis. It offers an essential source of information for decision-making in disease prevention and treatment. In several developed nations, certified genetic counseling professionals furnish this information to patients and their families. However, there’s a considerable shortage of such professionals in Asia, leading to a widespread lack of understanding about genetic diseases among patients. In 2018, the Genetic Counseling Branch of the Chinese Society of Genetics was established in China, and the body issued theACMG Genetic Variant Classification Standards and Guidelines. Since its inception, the branch has organized numerous training sessions in genetic counseling. Nevertheless, the confinement of genetic counseling services to only tertiary healthcare facilities impedes access and amplifies urban-rural disparities.
In conclusion, PGx is experiencing accelerated growth in China, providing an opportunity to engage young individuals with hypertension in primary healthcare settings. Despite policies promoting the use of PGx, there is a pressing need for hypertension management guidelines to embrace these advancements. The development of a learning-oriented primary healthcare service system, complete with tools to integrate genetic counseling into routine practice, is crucial in the Chinese context.
-
No conflicts of interest.
HTML
| Citation: |



 Download:
Download: